By Dr Sue Ferguson, Honorary Associate Lecturer at the School of Psychological Sciences, Macquarie University.
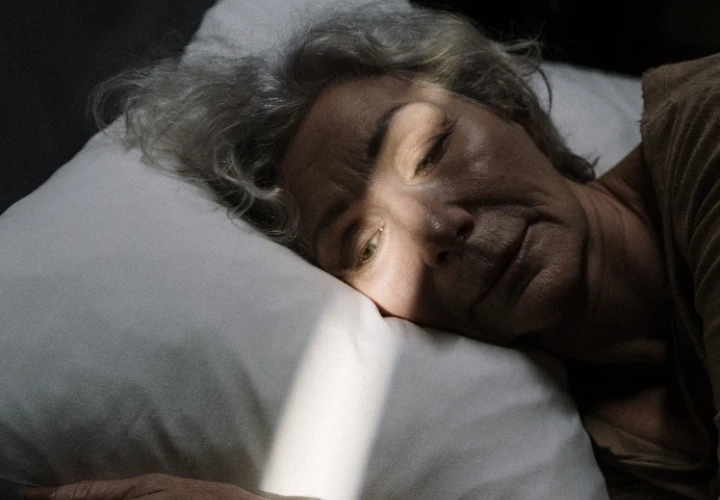
Several chronic physical illnesses, chronic pain, stress, anxiety, depression, and loneliness can each contribute to insomnia and poor-quality sleep with age, as can frequently nighttime urinating. Poor sleep is, in turn, associated with increased risk of falls in older adults, and contributes to further health risks, including cardiovascular disease, cognitive impairment, and higher mortality. This makes dealing with sleep problems, such as insomnia, more important than ever as we age. So, what changes in sleep occur with ageing? What are the most common sleep problems? How can you improve your own sleep? And where can you get more help and more information?
Changes in sleep as we age
From when we are aged in our 50s or 60s, there are several changes in sleep [1]: we tend to get sleepy earlier in the evening and wake up earlier in the morning (advanced sleep timing). With age we also take longer to get to sleep, have more frequent awakenings and increased time spent awake throughout the night (through difficulty getting back to sleep), and have a reduced amount of deeper restorative sleep (slow wave sleep), though most of these changes are more likely due to chronic illnesses rather than ageing itself. There has been debate about whether there is shorter overall sleep duration at night with older age (if there is, it’s possibly related to daytime napping, getting less exercise or chronic illness or pain). Note that adults, including older adults, only need about 7 (or up to 8) hours of sleep per night, so don’t spend too much extra time in bed if you are not sleeping.

Common sleep problems in older adults
Research suggests [2] that the most common sleep-related complaints of older persons are difficulty getting to sleep (and back to sleep) and daytime sleepiness or fatigue. The incidence of insomnia increases with age and is more frequent in women than in men. Although up to 50% of older adults report at least one symptom of insomnia, such as difficulty falling asleep, maintaining asleep, or early morning awakenings, a smaller percentage of older adults (5%–20%) met the diagnostic criteria for insomnia, which involves having symptoms at least 3 nights a week for at least 3 months, and having distress and/or impaired functioning in some areas of your life as a result.
Another common sleep issue involves excessive snoring and daytime sleepiness, if you have these symptoms, talk to your GP as you may need to be referred for a sleep study to check for Sleep Disordered Breathing (SDB) such as Obstructive Sleep Apnoea. SDB is a more common in older adults than younger adults and in men than women. Periodic Limb Movement disorder (such as restless legs) is also quite prevalent and both this and sleep apnea can disrupt your partner’s sleep too. Therefore, it’s definitely worth talking to your GP, and taking your partner with you (as they can help describe your sleep issues).
Improving your sleep
Research suggests these sleep tips (known as sleep hygiene) can help.
- Go outside in the morning (for some sunlight to help set your body clock)
- Get some exercise during the day (but not in the 3 hours before bed)
- Be careful not to nap too close to bedtime or for too long.
- Remove bright light and distractions from the bedroom (like TV or electronic devices)
- Don’t have caffeine after lunch, or alcohol or a large meal within 3 hours of bedtime.
- Develop a bedtime routine, like having a warm bath or hot drink, reading a relaxing book, or listening to soothing music or meditating.
- Try to go to bed and wake up at about the same time every day.
- If you wake for too long during the night, get out of bed for a while, do something relaxing, go back when you are sleepy.
Looking for support?
If you have tried these strategies and still have insomnia symptoms, talk to your GP, as sometimes sleep problems are caused by pain or other symptoms of chronic illnesses, or by the medications you are on, or you may have another sleep problem such as sleep apnea or restless legs or other sleep disorders. These can be investigated and often treated.
It is worth talking to your GP about medication and other options for insomnia, as there is new research on different drugs and other treatments [3] that might help. However, sleep medications [4] come with significant risks, so talk these over with your GP before taking these or any herbal remedies. Your GP might instead refer you to in-person treatment (with a psychologist) or help you through online cognitive behavioural therapy for insomnia (CBTi) [5]. Perhaps first you might like to try the Australian online cognitive behavioural therapy for insomnia program by This Way Up. It is well researched and free.
Want to know more?
Click here to visit the Australian Sleep Foundation website for more tips and resources.
Listen to an interview given by Australian sleep expert Dr Wai KUEN Chow, to Your Life Choices.
References:
[1], [2] Granter (2019) Sleep and Health. Ch4: Sleep and Health in Older Adults Academic Press- Elsevier
[3] Rosenberg, Citrome and Drake (2021) Advances in the Treatment of Chronic Insomnia: A Narrative Review of New Nonpharmacologic and Pharmacologic Therapies. Neuropsychiatric Disease and Treatment Neuropsychiatric Disease and Treatment 2021:17 2549–2566
[4] NPS Medicinewise (2015) Sleeping pills and older people: the risks
[5] Huang K, Li S, He R, et al. Efficacy of cognitive behavioral therapy for insomnia (CBT-I) in older adults with insomnia: A systematic review and meta-analysis. Australasian Psychiatry. 2022;30(5):592-597. doi:10.1177/10398562221118516